Human error in medicine
How AI and deep learning can overcome human error in medicine
Human errors in medicine are a stark reality. Research from Johns Hopkins Medicine estimated about 250,000 deaths a year in the US were due to inaccurate medical care, making it the third-leading cause of death (Makary et al., 2016).
Medicine is complex. There are complicated inputs, technical and physical limitations, all constrained by an at-times overburdened health system.
Disease diagnosis in radiology can be impacted by scan quality, but also challenges in interpretation.
A comprehensive research review found the retrospective error rate for radiological examinations was 30 per cent, with real-time errors estimated about 3 per cent to 5 per cent (Lee et al., 2013).
“Applying a 4 per cent error rate to the worldwide one billion annual radiologic studies equates to almost 40 million errors per annum,” the Insights Imaging report said.
Add in increasing workloads and systems at capacity and the error rate rises (Lee et al., 2013).
In this environment, artificial intelligence-based solutions increasingly provide accurate and consistent support for expert health professionals and medical specialists.
As AI and deep learning evolve, software can sometimes match human specialists in its accuracy for sensing, imaging, triaging or risk profiling tasks.
These technologies also have the capacity to deliver high-quality services at scale, potentially reducing barriers to healthcare for overburdened health systems in the developed world and underserviced hospitals in the developing world.
Amid skills shortages in radiology and other medical specialty areas, AI-enhanced decision-making has the potential to overcome key challenges in medicine and improve patient outcomes.
Here are some of the ways AI is supporting accuracy in healthcare and medicine.
Using AI in healthcare systems
AI and machine learning are proving to be highly accurate to support health professionals across a range of speciality fields.
AI uses large datasets to assess information, analyse patterns and make decisions. With deep learning, software can also use past experiences to predict outcomes instantly. And it never tires.
In medical care, AI-supported decision-making is being used for the detection of cancers, eye disease, stroke detection and coronary artery disease, among a range of other applications.
Rapid improvements in computer processes and deep learning are improving accuracy in radiology.
A study comparing deep learning algorithms to diagnose tuberculosis from chest X-rays found the best-performing AI model achieved 96 per cent accuracy (Ahuja, 2019). This was comparable to expert radiologists.
An AI software was reported to have higher accuracy than radiologists when assessing mammograms for breast cancer (Kim, 2020).
AI software is also supporting healthcare systems to meet demand. The CSIRO Patient Admission Prediction Tool is currently achieving about 90 per cent accuracy in monitoring and demand forecasting for healthcare services at Queensland hospitals.
The tool can predict how many patients will present to an emergency department and when, as well as forecast how many patients will require admission or discharge.
This assists patient flows and improves efficiencies across the system.
AI for coronary artery disease
AI is also proving beneficial in the assessment of coronary artery disease, one of the world’s leading causes of death and burden of disease.
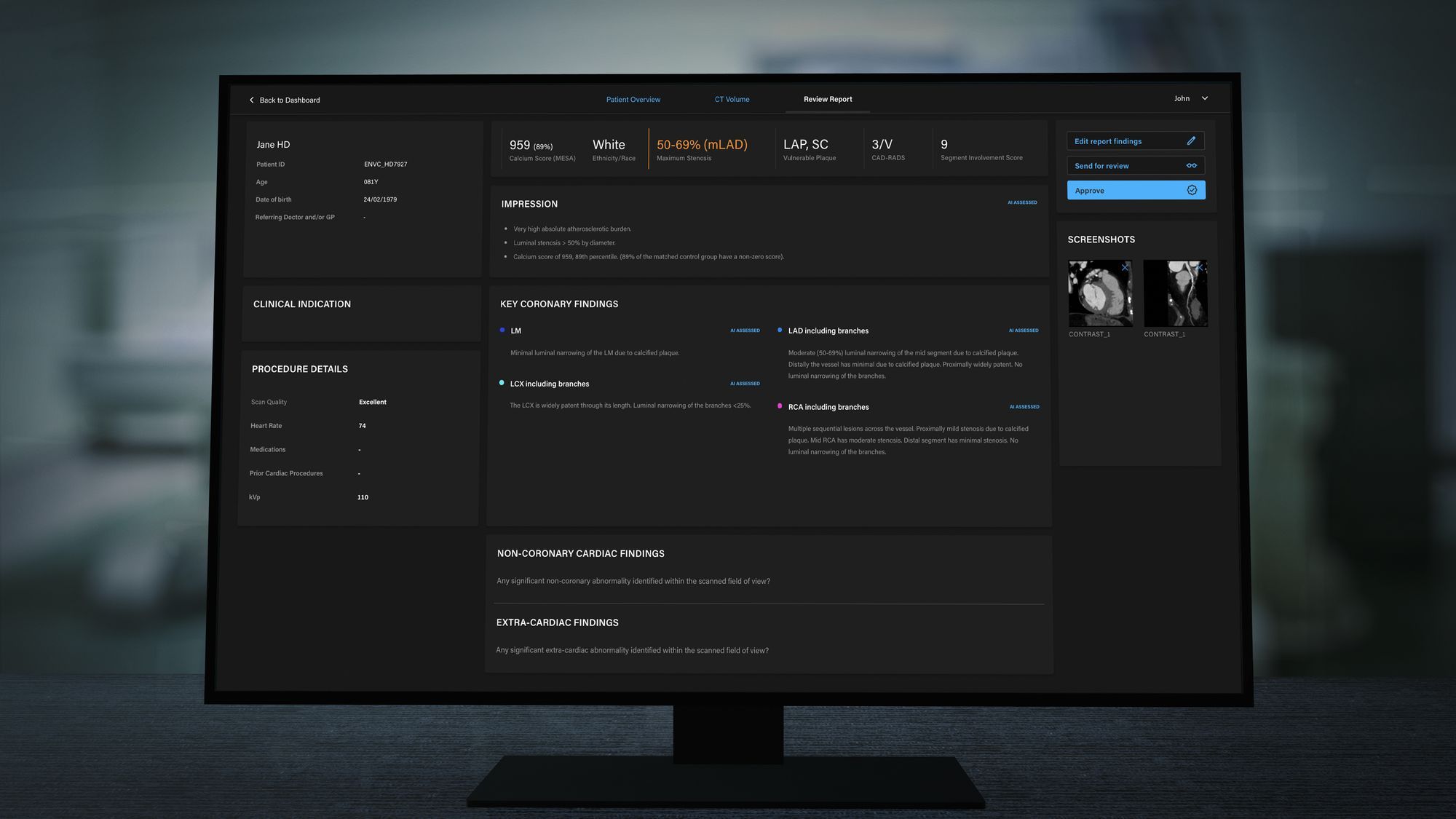
AI-based solution Artrya Salix can visualise multiple biomarkers of coronary artery disease accurately, within minutes.
The solution reports stenosis, calcification and, importantly, the presence of vulnerable plaque, to create a comprehensive picture of the coronary arteries. A growing body of research is pointing to vulnerable plaque as a critical predictor of major adverse cardiac events (Nerlekar et al., 2018).
But it is very challenging to detect vulnerable plaque. Finding and measuring soft plaque can be onerous and assessment can be subjective, which means experts do not always agree on its use in clinical practice. This highlights the potential for AI-assisted support for clinicians diagnosing coronary artery disease. Through internal studies, Artrya Salix detects and reports vulnerable plaque with accuracy greater than 70 per cent, providing meaningful data to support diagnoses.
Assisting expert decision-making
AI has the potential to improve medical care and overcome medical errors through reliable decision-making support.
Together with specialists to review and interpret AI-derived assessments, streamlined and consistent care can be provided.
A review from PeerJ said AI was tipped to play an increasing role in health and medical care (Ahuja, 2019).
“The rise of AI in the era of big data can assist physicians in improving the quality of patient care and provide radiologists with tools for improving the accuracy and efficiency of diagnosis and treatment,” the review said.
“The research firm Frost & Sullivan estimates that AI has the potential to improve patient outcomes by 30% to 40% while reducing treatment costs by up to 50%.”
“AI is well-suited to handle repetitive work processes, managing large amounts of data, and can provide another layer of decision support to mitigate errors.”
- Ahuja, A. “The impact of artificial intelligence in medicine on the future role of the physician”, PeerJ Life and Environment, October 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6779111/#ref-25
- Kim et al., “Changes in cancer detection and false-positive recall in mammography using artificial intelligence: a retrospective, multireader study” The Lancet, February 2020, https://www.thelancet.com/journals/landig/article/PIIS2589-7500(20)30003-0/fulltext
- Lee et al., “Cognitive and System Factors Contributing to Diagnostic Errors in Radiology”, American Journal of Roentgenology, September 2013, https://www.ajronline.org/doi/full/10.2214/AJR.12.10375
- Makary et al., “Medical error—the third leading cause of death in the US”, BMJ, May 2016, https://doi.org/10.1136/bmj.i2139
- Nerlekar et al., “Computed Tomographic Coronary Angiography-Derived Plaque Characteristics Predict Major Adverse Cardiovascular Events: A Systematic Review and Meta-Analysis”, Cardiovascular Imaging, January 2018, https://pubmed.ncbi.nlm.nih.gov/29305348